

Archived Insight | March 31, 2021
Get the health plan news you need for Q2 2021.
We cover:
Get the details below.

Share this page
Blue Cross Blue Shield published a report emphasizing that individuals with chronic conditions are significantly more vulnerable to COVID-19 than the general population and are three times more likely to be admitted to the intensive care unit.
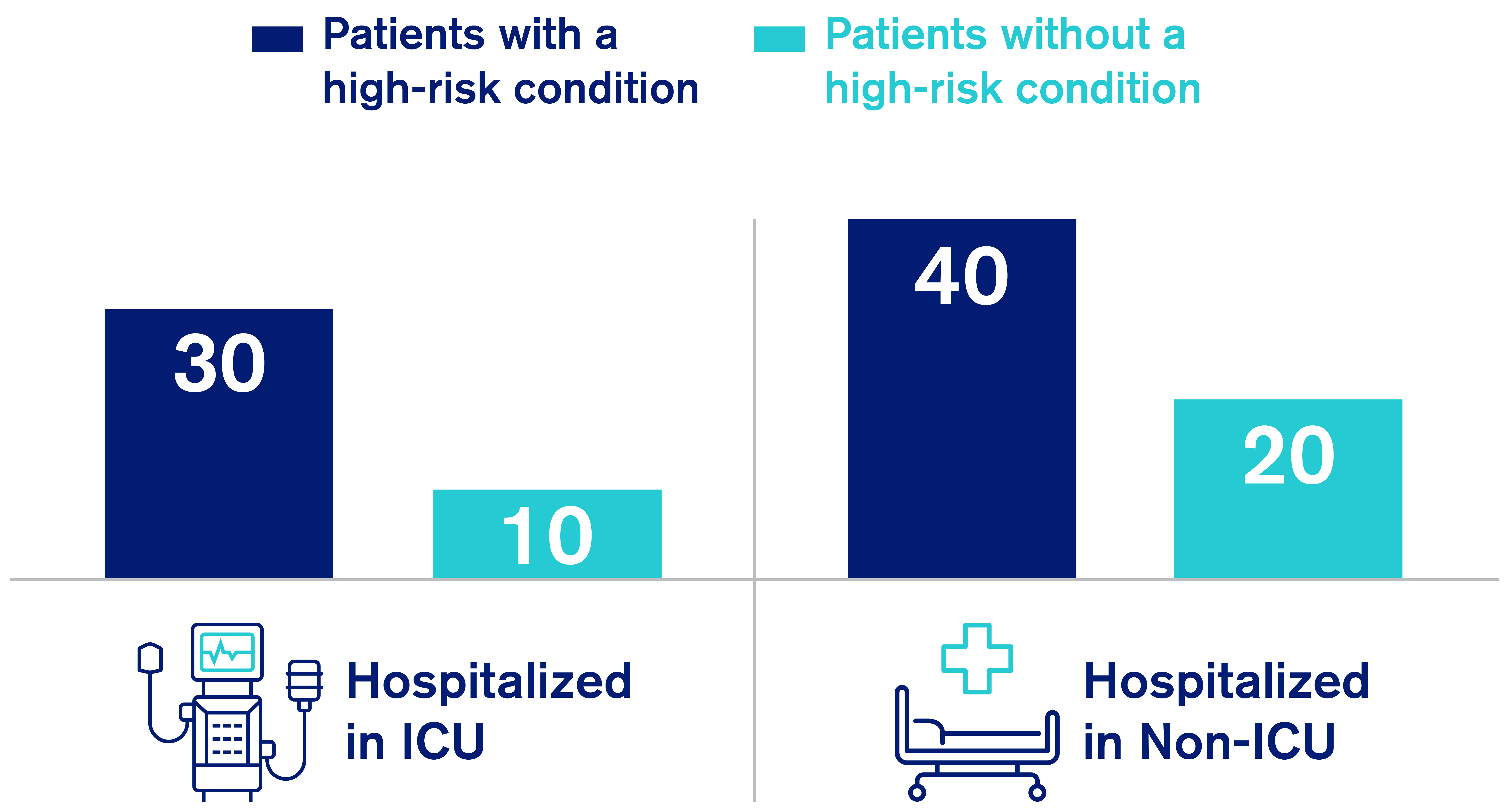
Source: Blue Cross and Blue Shield Association. “Infographic: COVID-19 patients with high-risk conditions 3x more likely to need the ICU.” Published February 9, 2021. Data reprinted with permission.
In the U.S., more than 10 percent of adults have diabetes and more than one-quarter of adults have pre-diabetes. Diabetic care is complex because additional health issues often accompany the disease.
Among the diabetic population:
Diabetics are also at an increased risk of worse health outcomes during the pandemic. COVID-19-related hospitalizations, ICU admissions and death rates are higher among diabetics than among non-diabetics. During the pandemic, 43 percent of diabetics that responded to an American Diabetes Association survey reported disruption in their care.
In addition, stay-at-home orders made it difficult to maintain healthy eating habits and regular exercise routines. Lastly, it is challenging for diabetics experiencing financial instability to afford healthcare and medication required to adequately manage their condition.
Diabetics who manage their condition well have a lower risk of developing a severe case of COVID-19 than those with poorly managed diabetes.
Plan sponsors may wish to implement and/or promote the following strategies for their diabetic population:
In 2019 (the latest data available), 7.4 percent of the U.S. population had a substance use disorder (SUD). Substance abusers often experience cardiovascular, pulmonary, metabolic and mental health issues and are at higher risk of overdosing and/or committing suicide.
SUDs are more common among the unemployed, poor and those living alone, all of which have increased due to COVID-19. Numerous reports indicate that substance use has increased and access to SUD treatment has decreased in the U.S. during the pandemic. Ten percent of adults reported increasing substance use to cope with stress.
Also, the CDC reported that the highest number of overdose deaths within 12 months occurred from June 2019 to May 2020, with the largest increase observed from March to May 2020. Additionally, ER visit rates for drug overdoses were higher from January to October 2020 compared to the same months in 2019. Furthermore, positive drug tests for illicit drugs have increased.
Because of the increase in SUDs and decrease in treatment availability, it is important for plan sponsors to focus their efforts on strengthening access to treatment.
First, promote the use of telemedicine to diagnose and treat SUD, and take advantage of virtual partial hospitalization and intensive outpatient programs that have emerged.
Second, ensure members struggling with opioid use disorder have access to medication-assisted treatment, which can help prevent relapses and overdoses.
Third, encourage members with SUD to attend virtual support programs, which can be helpful during recovery. Meetings, such as Narcotics Anonymous, have transitioned to an online format.
Our October 22, 2020 article provides more information about the adverse effects of SUDs and offers more solutions for how to prevent and address SUDs.
Plan sponsors should also ensure that behavioral health benefits are compliant with the Mental Health Parity and Addiction Equity Act.
The Consolidated Appropriations Act of 2021 requires plan sponsors to prepare an assessment of all behavioral health-related non-quantitative treatment limitations. Plans must provide this to the DOL or Health and Human Services (as applicable) upon request.
The Consolidated Appropriations Act of 2021 requires health plans to change how they pay for emergency services by 2022.
It also includes requirements such as prohibiting price “gag” clauses in contracts, requiring online search tools for participants to compare prices for care, and mandates that plans post files with their in-network rates, out-of-network allowable charges and prescription drug negotiated rates.
Plan sponsors should prepare to adopt these complex requirements by developing and implementing a comprehensive compliance strategy.
See details in our January 14 insight.
The HITECH Act amendment, which took effect on January 5, 2021, encourages covered entities and their business associates to follow “recognized security practices.” Adhering to these practices could result in lower fines or penalties, or shorter audits.
Learn more about this in our February 9 insight.
Starting April 1, 2021, the entire COBRA premium will be federally subsidized for six months. Employees (and their family members) that have already lost or lose health coverage due to job loss or reduced employment hours are eligible for this 100 percent subsidy.
This subsidy does not apply to individuals who have COBRA coverage due to voluntarily terminating employment.
It also does not apply when COBRA is triggered by other events such as death, divorce or a child aging out.
Read our March 11 insight for details.
To discuss the implications for your plan of
anything covered here, contact your Segal consultant or get in touch.

Compliance, Health, Multiemployer Plans, Public Sector, Healthcare Industry, Higher Education, Architecture Engineering & Construction, Corporate, Pharmaceutical

Technology, Benefits Administration, Communications, Multiemployer Plans, Public Sector, Healthcare Industry, Higher Education, Architecture Engineering & Construction, Consulting Innovation, Corporate, Benefits Technology, ATC, Organizational Effectiveness, Health, Retirement, Artificial Intelligence

Health, Compliance, Multiemployer Plans, Public Sector, Healthcare Industry, Higher Education, Architecture Engineering & Construction, Pharmaceutical, Corporate
This page is for informational purposes only and does not constitute legal, tax or investment advice. You are encouraged to discuss the issues raised here with your legal, tax and other advisors before determining how the issues apply to your specific situations.
Don't miss out. Join 16,000 others who already get the latest insights from Segal.
© 2026 by The Segal Group, Inc.Terms & Conditions Privacy Policy Style Guide California Residents Sitemap Disclosure of Compensation Required Notices