

Archived Insight | July 16, 2021
Get the health plan news you need for Q3 2021.
We cover:
Get the details below.
Medical cost trend (increase in allowed per capita claims cost) notably declined during the early months of the pandemic, but rebounded by the end of 2020, as shown by the graph below. Overall, medical costs in 2021 are expected to trend at similar rates observed pre-pandemic as people become more comfortable going to the doctor and catching up on delayed care.
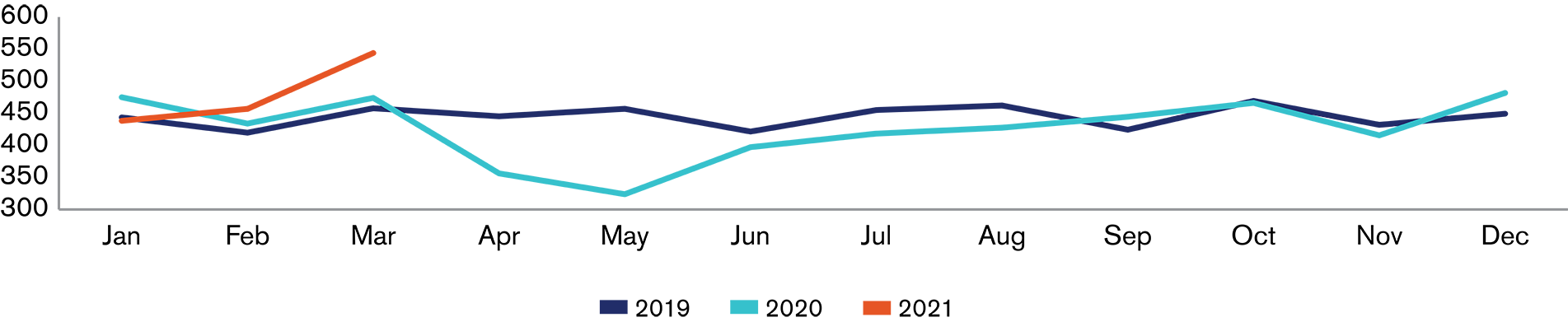
Source: Segal SHAPE database
The pandemic had an adverse impact on preventive cancer screening rates, as the graphs below illustrate. It remains to be seen what this lack of screening will mean for the severity of cancer cases in 2021 and beyond.








Preventive care is critical for maintaining and improving population health. The pandemic negatively affected utilization of preventive services. Consistent with the SHAPE data on the previous page, JAMA reported that 29 percent of U.S. adults missed a preventive visit during the first four months of the pandemic.
The deficit of preventive care is expected to cause long-term health consequences. Most notable is an increase in the number of conditions and diseases identified in later stages of progression. This could contribute to poorer health outcomes, higher morbidity and mortality rates and higher healthcare costs for plans.
Even prior to the pandemic, preventive services were underutilized. For example, although lung cancer is the leading cause of cancer death in the U.S., and despite evidence that lung cancer screening improves prognosis, it is estimated that compliance with lung cancer preventive screening is in the single digits.
Plan sponsors should ensure that their preventive benefits align with the most up-to-date recommendations. For example, the United States Preventive Services Task Force recently updated its lung cancer and colorectal cancer screening recommendations, both of which expand the eligible population. Additionally, plan sponsors should educate participants about the benefits of preventive services and consider implementing wellness benefits that incentivize use of preventive care. Lastly, plan sponsors should promote the use of virtual care as a point of access to preventive services.
The No Surprises Act, which includes provisions to protect patients from surprise billing by out-of-network providers, will be implemented starting January 1, 2022. Plan sponsors should work with their vendors to ensure that their health plans are compliant with the law’s new requirements.
Read about a recently released Interim Final Rule implementing the No Surprises Act.
The Biden administration recently announced that Section 1557 of the ACA, which prohibits group health plans from discriminating on the basis of sex, includes prohibiting discrimination on the basis of sexual orientation and gender identity. This reverses the Trump administration’s interpretation.
Read details on LGBTQ civil rights protections announced in May.
COVID-19 legislation enacted in 2020 includes tax credits for some employers who voluntarily provide paid sick and family leave for COVID-19-related reasons.
The IRS recently released guidance on how the American Rescue Plan paid leave tax credits work.
The Equal Employment Opportunity Commission released guidance that addresses whether employers are allowed to inquire about employees’ vaccination status and offer incentives to employees to get vaccinated. Federal equal employment law does not prohibit employers from requiring employees who are physically returning to the workplace to be vaccinated. Employers may also offer non-coercive incentives to obtain a vaccination.
Read more about how plans must cover COVID-19 vaccines without cost sharing.
To discuss the implications for your plan of
anything covered here, contact your Segal consultant or get in touch.

Compliance, COVID-19, Health, Mental Health

Health

Health, Technology, Public Sector
This page is for informational purposes only and does not constitute legal, tax or investment advice. You are encouraged to discuss the issues raised here with your legal, tax and other advisors before determining how the issues apply to your specific situations.
© 2024 by The Segal Group, Inc.Terms & Conditions Privacy Policy California Residents Sitemap Disclosure of Compensation Required Notices
We use cookies to collect information about how you use segalco.com.
We use this information to make the website work as well as possible and improve our offering to you.