

Archived Insight | January 11, 2021
Get the health plan news you need for Q1 2021. In this article we cover medical trends during the COVID-19 pandemic, plus strategies for managing costs.
We also round up the compliance information you need for your health plan in Q1 2021.
Share this page
Based on our analysis of SHAPE, Segal’s data warehouse, we’ve found that usage of a range of health services has changed because of COVID-19.
Compared to 2019, both use and cost of telehealth, substance use disorder and mental health services are higher during the pandemic. In contrast, use and cost of office and ER visits are lower.
Visits for substance use disorder are up 6% and mental health up 10%. As you might expect, office visits are 27% lower than in 2019. ER visits are down 23%.
(For more information, see our piece on digital trends during the pandemic, plus trends in telehealth use.)
* Read our April 14 insight and May 27 insight for context about the increase of telehealth use.


Learn about selected strategies for managing plans in Q1 2021 and beyond below.
 Cancer is the second leading cause of death in the United States and costs the healthcare system billions of dollars each year. Modifiable cancer-risk factors, such as tobacco use, alcohol consumption, excess weight, lack of exercise and exposure to UV light, are associated with 40 percent of cancer cases, as well as 50 percent of cancer deaths.
Cancer is the second leading cause of death in the United States and costs the healthcare system billions of dollars each year. Modifiable cancer-risk factors, such as tobacco use, alcohol consumption, excess weight, lack of exercise and exposure to UV light, are associated with 40 percent of cancer cases, as well as 50 percent of cancer deaths.
Early detection and diagnosis of cancer are critical for good health outcomes and lower-cost treatment. Late-stage cancer diagnoses are associated with poor health outcomes and intensive, high-cost treatments. The pandemic has adversely affected cancer detection and care in three major ways:
Breast, cervical and colorectal screening rates were more than 85 percent lower in March and April 2020 compared to their 2017, 2018 and 2019 rates. After April, the number of screenings increased; however, as of August 2020 (the latest data available), rates were still below 2019 levels.
According to a survey conducted by the American Cancer Society, 55 percent of cancer patients getting active treatment experienced some type of disruption in their care due to the pandemic.
Even before the pandemic, social determinants of health contributed to lower screening rates, higher incidence rates, higher frequency of late-stage diagnoses, higher mortality rates and lower-quality treatment among groups with poor or no access to cancer detection services and care. These groups include people historically discriminated against based on race, disability, sexual orientation, gender identity and other traits. The pandemic is worsening these disparities, as these groups are less able to access timely care.
Because of the pandemic’s negative impacts on cancer care, the American Association for Cancer Research projects an additional 10,000 deaths from breast and colorectal cancer during the next 10 years.
Plan sponsors should focus on strategies to combat these disruptions to cancer detection, care and treatment. Strategies include:
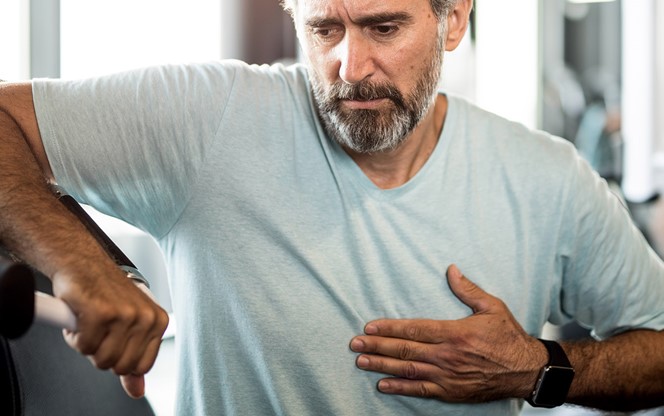
 Health plans closely monitor ER use due to the high costs associated with ER visits, as well as out of concern that some participants seek care at the ER for non-urgent medical conditions.
Health plans closely monitor ER use due to the high costs associated with ER visits, as well as out of concern that some participants seek care at the ER for non-urgent medical conditions.
As noted in the chart on page 1, the pandemic has changed ER use. Fear of exposure to COVID-19 may lead to deferred care even when patients should be seeking treatment for life-threatening conditions. The CDC reported that ER visits were 42 percent lower from March 29 through April 25, 2020 compared to the number of ER visits during the same time in 2019.
Of particular concern are studies reporting declines in ER use for truly urgent conditions, such as heart attacks and strokes. According to Epic Health Research Network, ER visits for those conditions were 45 percent and 38 percent lower, respectively, in late March/early April compared to pre-pandemic rates. JAMA, the Journal of the American Medical Association, also reported declines in ER visits for these conditions and an increase in number of non-COVID-19-related at-home deaths.
It is important to monitor these ER use patterns, as avoiding care for emergent conditions will result in worse health outcomes for participants and potentially higher costs for plan sponsors. As the pandemic continues, plan sponsors should educate participants about the appropriate uses of telemedicine, urgent care and the emergency room, respectively, and encourage participants to use the ER only for truly urgent situations. Additionally, plan sponsors should continue to expand and promote the use of telemedicine. Participants can use telemedicine to triage their symptoms and determine if a trip to the ER is necessary.
We cover information related to COVID-19 vaccines, as well as the new transparency rule and mental health parity tool.
The DOL and HHS released new guidelines regarding the coverage of COVID-19 preventive services, such as vaccines. Non-grandfathered group health plans will be required to cover COVID-19 vaccines in-network at no cost to the member. During the Public Health Emergency, vaccines must be covered without cost regardless of provider network status.
Read more about the coverage of preventive services and learn about vaccine coverage specifically.
The final transparency rule requires non-grandfathered group health plans to publish publicly negotiated rates for in-network providers, as well as allowed amounts for out-of-network providers. The final rule also requires these plans to provide cost-sharing information to plan participants before they receive healthcare services.
Read more details about transparency requirements.
The DOL and HHS recently released a tool that will help plan sponsors determine their level of compliance with the Mental Health Parity and Addiction Equity Act.
Get more information about the tool.
From the implications of the pandemic to plan management, Segal has you covered.
To discuss the implications for your plan of anything covered here, get in touch.

Health, Compliance, Multiemployer Plans, Public Sector, Healthcare Industry, Higher Education, Architecture Engineering & Construction, Pharmaceutical, Corporate

Compliance, Health, Multiemployer Plans, Public Sector, Healthcare Industry, Higher Education, Architecture Engineering & Construction, Pharmaceutical, Corporate

Health, Compliance, Multiemployer Plans, Public Sector, Healthcare Industry, Higher Education, Architecture Engineering & Construction, Corporate
This page is for informational purposes only and does not constitute legal, tax or investment advice. You are encouraged to discuss the issues raised here with your legal, tax and other advisors before determining how the issues apply to your specific situations.
© 2024 by The Segal Group, Inc.Terms & Conditions Privacy Policy California Residents Sitemap Disclosure of Compensation Required Notices
We use cookies to collect information about how you use segalco.com.
We use this information to make the website work as well as possible and improve our offering to you.