

Articles | July 27, 2022
Over the last several decades, a wave of innovative new drug therapies came to market that improved and even extended millions of lives. They also came with enormous price tags that have made prescription drug benefits an important part of the health benefit package your plan participants depend upon.
Many plan participants use their prescription drug coverage each year. The benefits need to be responsive to their clinical and logistical needs. The coverage must also be affordable.

Share this page
Achieving the goal of delivering cost-effective prescription drug coverage to plan participants is increasingly challenging because there are numerous cost drivers. To get more mileage from prescription drug benefits, plan sponsors need to pay close attention to each of the following:
This article discusses these important aspects of prescription drug cost management, as well as providing an overview of cost drivers.
In the 1980s, most health insurance plans covered outpatient drug claims under their medical plan insurer, like all other medical services, such as hospital and surgical benefits. Outpatient prescription drugs were subject to the medical plan deductibles and coinsurance requirements. They represented about 4 percent of total medical plan spending, while hospital claims consumed up to 50 percent of a typical medical benefit plan budget. Medicare didn’t cover outpatient prescription drug claims, and pharmacy benefit managers were just arriving on the scene with promises of easy access to medications and plan savings.
Today, outpatient prescription drugs now account for 20 to 25 percent of the typical overall medical plan cost spending and are the second-highest segment of plan sponsor expenses, after inpatient hospital claim costs.
PBMs have expanded their services beyond claims processing to include more sophisticated drug utilization review and formulary options to drive better drug pricing.
In any given year, 35 to 50 percent of a plan’s active covered population will have at least one prescription drug claim. For retiree plans, the range jumps to 80 to 90 percent of the covered population. In contrast, only about 7 to 8 percent of plan participants will be admitted to the hospital in a year. Further, the average claimant has about eight outpatient Rx claims per year.
Unfortunately, the prescription drug industry is plagued with many problems, including — but not limited to — massive marketing efforts and protective federal laws that extend patents, permit rebate schemes and allow other anti-competitive tactics that increase plan costs. PBMs add to the problem with their lack of transparency and complicated contracting schemes that can generate higher costs. Finally, wasteful prescribing patterns by some physicians adds to the system’s excess costs.
The result: Americans spend more than twice as much per person per year for outpatient drugs than most other industrialized nations with lower life expectancy rates.
Even as we wait for meaningful federal policies to lower drug costs to patients, plan sponsors can significantly reduce their prescription drug benefit plan costs while improving the effectiveness of the outpatient prescription benefits. To be able to do this, plan sponsors need to understand the cost drivers.
These are among the most significant plan cost drivers:
Effective prescription drug plan designs address these questions:
The answers depend on many factors, including the income levels of the workforce, the plan sponsor’s industry and budgetary constraints.
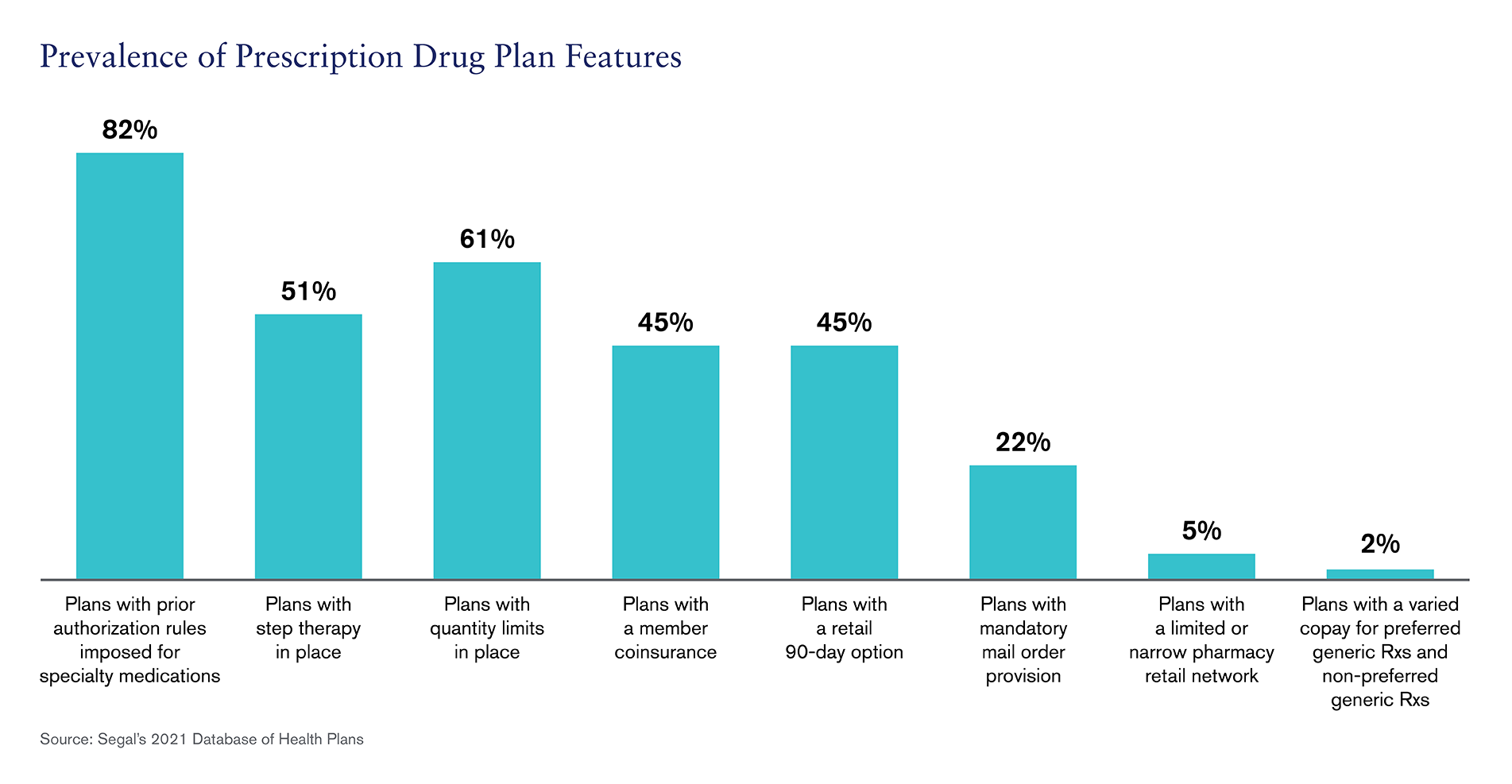
The graph below shows the prevalence of some prescription drug plan features currently being used by plan sponsors.
These five strategies are among the best practices for managing the cost of prescription drug coverage:
Price setting for pharmaceuticals is a complicated process. It’s important to recognize that the actual “sales price” of a prescription drug varies dramatically by buyer and on average is somewhere between 50 percent to 55 percent of the actual “list price of drug.” The actual production costs to produce a drug may be only 15 percent of the typical revenue earned by a manufacturer.
As a result, there is a lot of room for drug manufacturers to create complex pricing schemes and incentives to improve their market share, while still enjoying high profit margins. Of course, drug companies will need revenue to cover more than production, distribution and marketing costs, and costs to recoup research and development.
The large gaps between revenue and costs means there’s an opportunity for plan sponsors to negotiate better pricing. Plan sponsors need to recognize their buying power. By understanding the best prices available in the market and the true breakeven operating expenses of PBMs and retail pharmacies, plan sponsors can trade market share for better pricing in contracts and cut out much of excess margins retained by the intermediaries (e.g., PBMs, retail pharmacies and mail-order pharmacies).
Consider these PBM contract RFP must-haves:
Applying more rigor to a PBM contract and RFPs can result in substantial annual savings to the plan and the plan participants — without compromising benefit value.
Prescription drug benefits involve more than cost.
There is tremendous value in a strong PBM partner that provides meaningful clinical support to your plan participants. Knowledgeable and responsive clinical staff can help guide you to programs or strategies that improve patient quality of life.
Not all PBMs are the same. Plan sponsors should test the PBM’s clinical systems and staff and only use the programs that will work for the plan. In some cases, utilization management programs, like prior authorization and step therapy, are useful tools to produce plan cost savings. In other cases, clinical programs that support participants who have complex needs and conditions may not save on the prescription drug claim costs but can avoid costly medical plan claims and complications. Turning on the right clinical programs can make a difference in patients’ quality of life and appropriate physician prescribing.
An expert review of the PBM clinical program offerings is an essential step to creating programs that avoid needless burdens and inconveniences to your plan participants as well as providing worthwhile value to your plan.
Prescription drug benefits are an essential, high-touch benefit for most plan participants. The programs are highly valued by participants and their dependents and require the proper due diligence.
By applying the tools and strategies to this benefit, plan sponsors can provide cost-effective prescription drug benefits.
Let’s discuss a strategy.
Get in Touch
Health

Health, Multiemployer Plans, Public Sector, Corporate, COVID-19

Health, Compliance
This page is for informational purposes only and does not constitute legal, tax or investment advice. You are encouraged to discuss the issues raised here with your legal, tax and other advisors before determining how the issues apply to your specific situations.
© 2024 by The Segal Group, Inc.Terms & Conditions Privacy Policy California Residents Sitemap Disclosure of Compensation Required Notices
We use cookies to collect information about how you use segalco.com.
We use this information to make the website work as well as possible and improve our offering to you.