

Articles | June 8, 2022
Our latest short quarterly roundup of healthcare news for plan sponsors covers:
Get the details below.
The pandemic disrupted medical costs and utilization trends for two years. The graph illustrates utilization patterns from 2019 through 2021 for different sites of care.
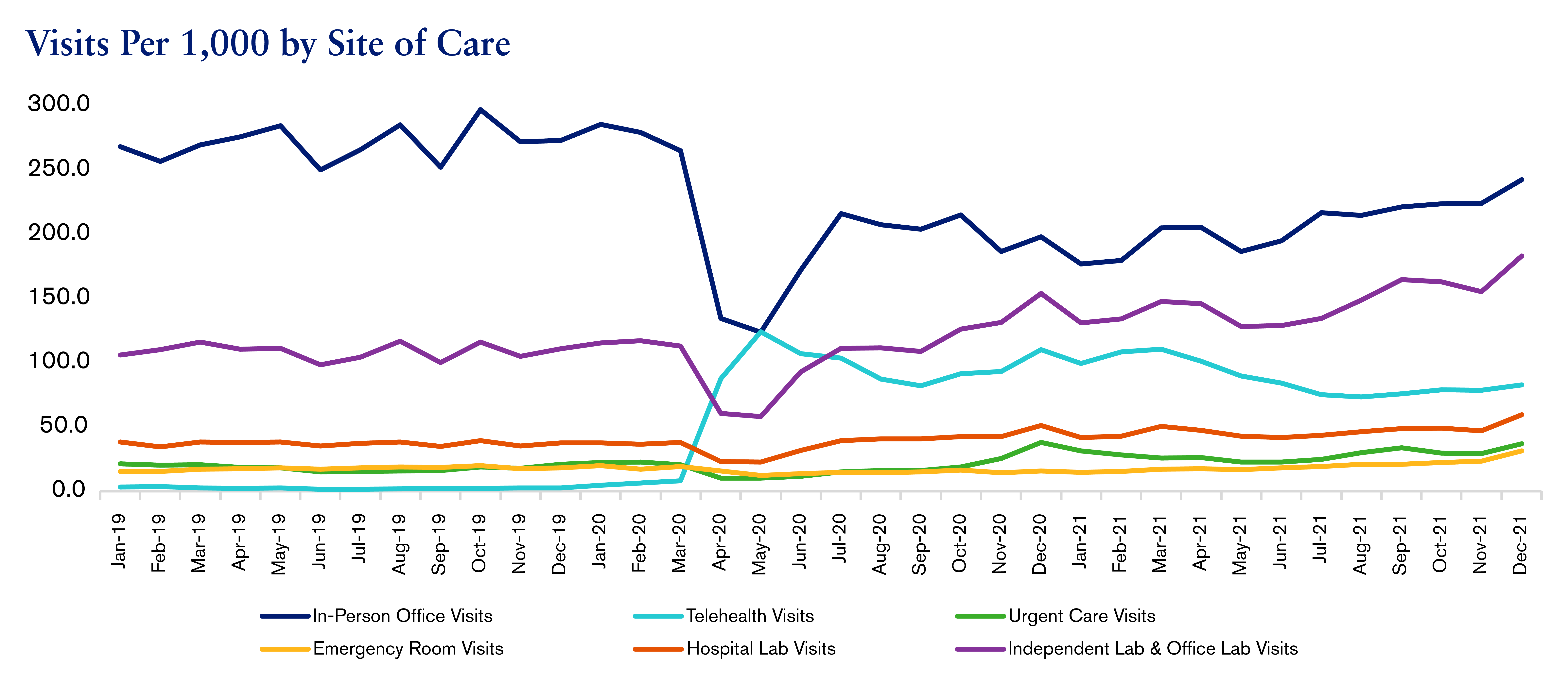
Utilization trends shifted during the pandemic, as in-person care was not always available and patients avoided hospitals out of fear of contracting COVID-19. In the past two years, care has notably shifted away from high-cost settings, such as inpatient hospitals and emergency rooms (ER), towards low-cost settings, such as telehealth, urgent care centers and the home. This pattern is expected to continue.
At the beginning of the pandemic, inpatient admission rates and ER rates declined significantly. In 2020, admits and ER visits were lower than expected. However, cases treated in these settings were more severe than those treated before the pandemic.
Conversely, urgent care and telehealth visits markedly increased. COVID-19 testing and vaccine administration were two of the most common reasons to visit an urgent care clinic, while mental health and substance use disorders were the top two conditions treated via telemedicine. Telehealth played a critical role in expanding and maintaining care during the pandemic. Despite the technological barriers of virtual care and concerns about both the quality of care provided and equitable access, it has the potential to transform treatment, especially for behavioral health and chronic condition management.
Home-based care has evolved as well. At-home care is expected to increase in the coming years because it’s convenient, especially for elderly patients and for those with complex comorbidities. Some providers are conducting home visits as follow-ups to virtual care visits, when in-person care is needed.
In-person office visits have been lower than expected, as patients opt for virtual visits; additionally, an increasing number of patients don’t have a primary care physician (PCP). An in-person office visit is a low-cost option that can be used instead of an emergency room or urgent care center for non-emergent medical issues. However, it’s also beneficial to participants’ health to have an established relationship with a PCP.
It’s important for participants to understand site-of-care options so they can seek and receive the correct level of care. Plan sponsors can educate participants on the appropriate use of different treatment settings. For example, urgent care centers are good alternatives to the ER in non-emergent situations, but an urgent care visit shouldn’t replace a PCP in-person office visit.
Plan sponsors can also modify benefits and plan design to encourage participants to seek care in lower-cost settings. Plans can implement higher cost sharing for certain hospital-based visits, including lab visits, and lower cost-sharing for telehealth, in-person office, urgent care and independent lab visits.
Lastly, plan sponsors should invest in virtual health services. Plans can incorporate virtual primary care and urgent care services into benefit offerings, as well as adopt digital tools to facilitate physicians’ ability to better manage, monitor and coordinate participants’ care.
The Coronavirus Aid, Relief and Economic Security (CARES) Act included a safe harbor that allowed high-deductible health plans (HDHPs) paired with health savings accounts (HSAs) to cover telehealth before participants met the deductible, effective through December 31, 2021. The Consolidated Appropriations Act of 2022 extended this coverage for telehealth services incurred between April 1, 2022 and December 31, 2022. Plan sponsors should confirm that telehealth benefits for HDHPs with HSAs are being administered properly.
Learn more about this in our March 22 telehealth exemption insight.
There are many components to the No Surprises Act, including the transparency laws and surprise medical billing rules. Plan sponsors should ensure their plans comply with these rules and deadlines.
See details in our April 14 insight covering surprise billing.
Contact your Segal consultant or get in touch with us.

Health

Health

Health
This page is for informational purposes only and does not constitute legal, tax or investment advice. You are encouraged to discuss the issues raised here with your legal, tax and other advisors before determining how the issues apply to your specific situations.
© 2024 by The Segal Group, Inc.Terms & Conditions Privacy Policy California Residents Sitemap Disclosure of Compensation Required Notices
We use cookies to collect information about how you use segalco.com.
We use this information to make the website work as well as possible and improve our offering to you.